Dear All (with thanks to Kevin Outterson for leading this note),
HUGE news today: Senator Michael F. Bennet and Senator Todd Young have introduced an updated PASTEUR Act that (if enacted) would create a predictable path to rewarding new #FireExtinguishersOfMedicine for their value to society via a subscription contract (valued at $750m to $3b) that prepays for all US federal use of the drug. This is a delinked pull incentive that is large enough to move the R&D needle, with powerful support for antibiotic stewardship. Bravo!
The full bill is here (link), the one-pager for the bill is here (link, the text of the one-pager is also copied below our signatures), and (iii) a set of FAQs that we created. The key concepts are:
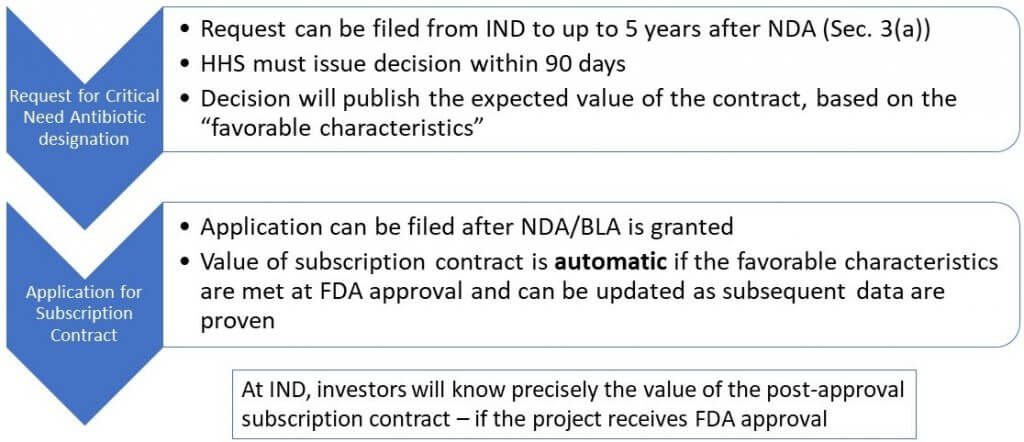
- At IND (or a later time of the sponsor’s choosing), the innovator can request designation as a Critical Need Antibiotic based on anticipated product properties. By this, investors will know precisely the potential value of the post-approval subscription contract from the US that will automatically be granted if the project receives FDA approval.
- The value will be in the range $750m to $3b based on the product attributes that are actually achieved.
- Smaller transitional awards can be made while the system is being set up.
- Hospitals get financial support to improve diagnostics and stewardship.
- A $11b fund is created to pay for the first wave of these antibiotics; a rolling review process (and renewal, we hope!) is implied by the Act.
This graphic gives a bit more detail:
Wow! This dovetails perfectly will the global benchmark value of up to $4b set by the UK with its pilot subscription model (link to 29 Mar 2020 newsletter).
We’re sure there will be lots of discussion in the coming days on this proposed legislation (comments are invited at AMR@bennet.senate.gov — and we suggest that a simple “THANK YOU!” would be a great note to send all by itself), but it is a huge step in the right direction!
Senator Bennet said: “We are living through the worst pandemic in a century, and infectious disease experts are sounding the alarm that drug-resistant bacteria will lead to another public health crisis. The PASTEUR Act would provide antibiotic researchers and developers with the resources and certainty they need to prepare for the threat that resistant infections pose. Our bipartisan legislation will better arm hospitals and providers in the fight against antimicrobial resistance by incenting development, targeting the most threatening infections, and encouraging the appropriate use of antibiotics.”
And as Senator Young said, “Antimicrobial resistance has become a growing crisis in recent years. Market failures have resulted in a lack of needed research and development in this field which is a threat to public health. That’s why I am proud to be working with Senator Bennet to introduce the Pioneering Antimicrobial Subscriptions to End Upsurging Resistance (PASTEUR) Act to incentivize development of new antibiotics. At the same time, the PASTEUR Act will focus on educating health care providers on how to avoid overuse or misuse of these life-saving medications in order to slow the emergence of antibiotic-resistant pathogens.”
With thanks to Senators Young and Bennet and all best wishes to the R&D community, Kevin and John
PS: Be sure to also look at the meetings calendar: there is a newly posted R&D Bootcamp webinar on pre-clinical safety assessments!
Kevin Outterson, JD, Professor of Law, Boston University & Executive Director, CARB-X (these views are personal and do not necessarily reflect the views of CARB-X or any of its funders) @koutterson
John H. Rex, MD | Chief Medical Officer, F2G Ltd. | Operating Partner, Advent Life Sciences. Follow me on Twitter: @JohnRex_NewAbx. See past newsletters and subscribe for the future: https://amr.solutions/blog/. All opinions are my own.
Text from the one-pager for the PASTEUR Act (link): The Pioneering Antimicrobial Subscriptions to End Upsurging Resistance (PASTEUR) Act establishes a delinked subscription program to encourage innovative antimicrobial drug development targeting the most threatening infections, improve the appropriate use of antibiotics, and ensure domestic availability when needed.
Establishment of Subscription Model for Critical Need Antimicrobials:
- The Secretary of the Department of Health and Human Services (HHS) will appoint a new ‘Committee on Critical Need Antimicrobials’ with representatives from relevant federal agencies.
- The HHS Secretary will appoint an ‘Critical Need Antimicrobials Advisory Group’ including patient advocates and outside experts.
- HHS and the Committee, with support from the Advisory Group, will identify infections to help target novel antimicrobial development, select an office or agency to manage the subscription program, and develop regulations and guidance determining monetary valuation and terms of subscription contracts.
- Contract value will be determined by evidence-based preferred drug characteristics to incentivize development of innovative antibiotics.
- Contracts will be fully delinked and payments will be adjusted down by any amount Federal health programs pay for the drug.
Transition Measures:
- During a transition period, the HHS Secretary, through an appropriate office or agency, may use funding to enter into smaller contracts with companies developing innovative antimicrobial drugs.
- Transitional contracts will include terms of participation, including developing appropriate use strategies, the completion of FDA-required post-marketing studies, and a reliable supply chain.
Critical Need Antimicrobial Designation and Valuation:
- An antimicrobial drug developer can apply to receive a ‘critical need antimicrobial’ designation. HHS will evaluate whether the drug meets preferred characteristics and determine the drug’s subscription contract eligibility and value.
- A drug developer may apply to HHS for a subscription contract at or within five years following FDA approval. Contracts will range from $750 million to $3 billion and will be paid out over a period of up to 10 years or through the length of patent exclusivity. In return, patients covered by federal insurance programs will receive these drugs at no cost.
- HHS and manufacturers can negotiate smaller secondary contracts to extend subscription plans or, in the case of new post-market information, adjust the value of subscription plans.
Subscription Contract Terms, Conditions, and Appropriate Use:
- Drug developers must adhere to certain requirements, including ensuring product availability, tracking resistance data, supporting appropriate use, and post-marketing studies.
- The Secretary will work with the Advisory Group and professional societies to develop timely clinical guidelines for using critical need antimicrobials.
- Providers will be encouraged to report antibiotic use through the CDC National Healthcare Safety Network Antimicrobial Use and Resistance module and other programs to improve appropriate use.
- HHS and the CDC will use health surveillance systems to collect and report on antibiotic use and resistance data.
Funding and Reports:
- Congress will provide $11 billion to support the program over 10 years.
- Within six years, the Government Accountability Office will conduct a study on the program’s effectiveness and will be sent to Congress.
- The CDC will conduct annual reports on Antibiotic Use in the United States and reports on both antifungal resistance and antimicrobial prophylactics, like vaccines.
FAQs (created by Kevin & John):
- Who makes the decisions about issuing the subscription agreements? After the FDA approves a drug or biologic that holds a Designation as a Critical Need Antibiotic, the sponsor can apply for the subscription contract and will automatically receive the pre-set dollar values (adjusted for inflation) that were published in the Designation, but only for the favorable characteristics actually achieved at FDA approval or subsequently.
- What are those favorable characteristics? This will be determined by a HHS regulation within a year, but PASTEUR gives clear guidance that these should generally be things that a preclinical program can target: being active vs. a priority pathogen, being a novel class or mechanism of action, targeting a difficult to reach body site, or having a certain route of administration. For ideas on what we hope to see here, see also these sources:
- Our 2016 article in Lancet ID (link). Entitled “Antibiotic reimbursement in a model delinked from sales: a benchmark-based worldwide approach,” this paper proposed value based on defined attributes (e.g., nature of the target, spectrum, PO vs. IV, etc.).
- The UK subscription pilot (link to 29 Mar 2020 newsletter). The UK is using a point-based system to determine value — in the newsletter, search for ‘ranking’ to jump to the text the gives details on the UK’s thinking.
- How long is the subscription contract? The longer of 10 years or the patent/exclusivity length for the product in the FDA Orange Book.
- What revenues are replaced by the subscription contract? The subscription contract covers all federal uses – Medicare, Medicaid, VA, CHAMPUS, TRICARE, Indian Health Service, etc. Subscription contract payments are adjusted down by the same amounts that sponsors receive as revenue from these programs.
- What about private US and global sales? These are not covered by the subscription contract, so the company keeps any revenues from these sources.
- What types of antimicrobials are eligible? Antibacterial therapeutics only (no anti-fungals), whether a drug or biologic.
- How does this help stewardship? Companies signing a subscription contract agree to high standards of stewardship. As a delinked pull incentive, the company doesn’t have any incentive to overmarket. The Act also allocates $500m to support hospital use of diagnostics and stewardship.
- What are the Transitional awards? Drafting and approving the regulations and setting up the Office will take at least a year, so the Act allows HHS to make some transitional awards in the interim.
Current funding opportunities (most current list is here):
- Novo REPAIR Impact Fund closed its most recent round on 31 Jul 2020. Go here for current details.
- 2020 funding rounds for CARB-X have not been announced.
- The Global AMR R&D Hub’s dynamic dashboard (link) summarizes funders and projects by geography, stage, and more.
- It’s not a funder, but AiCuris’ AiCubator offers incubator support to very early stage projects. Read more about it here.
- You might also be interested in the most current lists of R&D incentives (link) and priority pathogens (link)
Upcoming meetings of interest to the AMR community (most current list is here):
- [Registration is now open] 2 Oct 2020 (online meeting): 7th annual Boston Area Antimicrobial Research Network (BAARN) meeting. Go here for details on this (free!) online meeting.
- [NEW] 8 Oct 2020 (online, 16.30-18.30 CEST; 10.30a-12.30p EST); Bootcamp #2 entitled “Exploring safety issues in antimicrobial drug development”. Moderated by Claire Sadler (Apconix), this webinar is jointly sponsored by GARDP, CARB-X, Novo REPAIR, JPIAMR, Wellcome Trust, ASM, and ESCMID. Since we can’t the ASM-ESCMID meeting, we’re still going to have the bootcamps! Go here to register.
- 21-25 Oct 2020 (online meeting), IDWeek 2020. Go here for details.
- 26-29 Oct 2020 (online meeting), Annual ESPID meeting (European Society for Pediatric ID, #38)
- 27 Oct 2020 (online, 9a-5p EST): FDA Workshop entitled “Development Considerations of Antimicrobial Drugs for the Treatment of Gonorrhea.” Go here to register.
- 27 Oct 2020 (online meeting), BARDA Industry Day, a discussion of U.S. Government medical countermeasure priorities. Mark your calendar now and watch this website for details.
- 18-24 Nov 2020 (everywhere): World Antimicrobial Awareness Week. For resources, go here for WHO’s home page for the week. The focus will be on two messages: “Antimicrobials: handle with care” and “United to preserve antimicrobials.”
- 9-12 Jul 2021 (Vienna): Annual ECCMID meeting (#31)
- 18-21 May 2021 (Albuquerque, New Mexico): Biannual meeting of the MSGERC (Mycoses Study Group Education and Research Consortium). Save-the-date announcement is here, details to follow.
- 20-24 June 2021 (Toronto): International Symposium on Pneumococci and Pneumococcal Diseases (ISPPD-12). Go here for details.
- 3-7 Jun 2021 (Anaheim), ASM Microbe 2021. Go here for details.
- 27 Jun-2 Jul 2021 (Ventura, CA): Gordon Research Conference entitled “Antimicrobial Peptides”. Go here for details, go here for the linked 26-27 Jun Gordon Research Seminar that precedes it.
- 5-21 Aug 2021 (Marine Biology Laboratory, Woods Hole, MA): Residential course entitled “Molecular Mycology: Current Approaches to Fungal Pathogenesis.” This 2-week intensive training program has run annually for many years and gets outstanding reviews. Go here for details.
- 8-11 Oct 2021 (Aberdeen, Scotland): 10th Trends in Medical Mycology. Go here for details.
- 16-24 Oct 2021 (Annecy, France): Interdisciplinary Course on Antibiotics and Resistance (ICARe). This is a soup-to-nuts residential course on antibiotics, antibiotic resistance, and antibiotic R&D. The course is very intense, very detailed, and gets rave reviews. Registration is here and is limited to 40 students.
- 6-11 Mar 2022 (Il Ciocco, Tuscany): Gordon Research Conference entitled “New Antibacterial Discovery and Development”. Go here for details, go here for the linked 5-6 Mar Gordon Research Seminar that precedes it.