Dear All (with thanks to Vega Masignani for co-authoring this newsletter),
While the work needed to create new antibacterial agents is the primary topic of this newsletter, the need for vaccines of all types is definitely part of our community’s joint remit. As discussed in the 29 Mar 2021 newsletter (“Vaccines to turn back the tide of antimicrobial resistance”) with further insights on key challenges in the 21 Jul 2025 newsletter (“Vaccination to prevent AMR: Insights from Wellcome”), viral infections often result in the inappropriate use of antibiotics—either due to misdiagnosis or precautionary prescribing—which fuels resistance. Moreover, viral infections may pave the way to bacterial infections. This means that vaccines for both viral and bacterial infections help reduce AMR. In short, the best way to not need an antibiotic (of any type) is to prevent the infection in the first place.
And, of course, the overall impact of vaccines is enormous. Although it can be difficult to prove the impact of specific vaccines in a detailed fashion (21 Jul 2025 newsletter mentioned above), a recent WHO-led paper (Carter et al., Vaccine 2024, doi:10.1016/j.vaccine.2023.07.03, concluded that vaccines will prevent more than 50 million deaths worldwide during this decade (2021-2030).
But, vaccine development (like drug development) is a long, hard, expensive, and failure-prone process. Despite the number of new products remaining stable over the last 30 years, the associated R&D costs have multiplied thus creating an imbalanced situation between the investments required and the expected turn-over of a product – namely, the so-called “productivity gap” (see Pronker ES et al., PLOS One 2013, doi: 10.1371/journal.pone.0057755).
Although the SARS-CoV2 pandemic was a transformative event in vaccine R&D that showed the potential for dramatic innovation (see Sabow et al., McKinsey Life Sciences 2024), the impact of the new insights has been uneven across disease areas. Targets for emerging infections and nosocomial pathogens remain neglected, thus resulting in global vaccine inequity and persisting serious public health challenges (see 9 Nov 2022 WHO press release and report: “WHO releases first data on global vaccine market since COVID-19”). As the bulk of the costs for developing novel products is mainly due to the cost of (large!) Phase 3 studies, strategies to de-risk vaccine candidates as early as possible during clinical development would make a real difference.
On this specific point insights gained over the past > 50 years have validated multiple de-risking strategies: (i) Correlates of Protection (CoP), (ii) controlled human infection models (CHIMs), and (iii) early, focused studies in higher-risk populations. As a summary of the lessons learned, we have this new paper:
- Masignani, V., Palacios, R., Martin, MT. Tibaldi F, and Vadvelu VK. De-risking vaccine development: lessons, challenges, and prospects. npj Vaccines 10, 177 (2025). https://doi.org/10.1038/s41541-025-01211-z.
Before we begin our tour of the paper, let’s take a moment to consider the most obvious way you might show that a vaccine prevents infection. Given that infections occur randomly and (we hope) in a only a few percent of the population, you may need to immunize thousands (or even tens of thousands) of individuals to show an effect. This is obviously slow and expensive! And in some extreme cases, the incidence of a given disease is so low in the general population that Ph3 efficacy studies are in fact impossible to execute. So, what can you do to simplify the process and confirm early in development that your product has an effect? As discussed in the paper, three ideas are available:
1. Correlates of Protection (CoP): When immunity is based on the amount of antibody produced to a given antigen, your blood levels of these specific antibodies (“the antibody titer”) can be correlated with likelihood of protection from the disease. No antibody = no protection (of course), and then careful, lengthy, and complex work can ultimately establish that (say) 0.35 μg/mL of antigen-specific IgG is protective (as is the case of polysaccharide-conjugated vaccines for Streptococcus pneumoniae, aka, ‘the pneumococcus’).
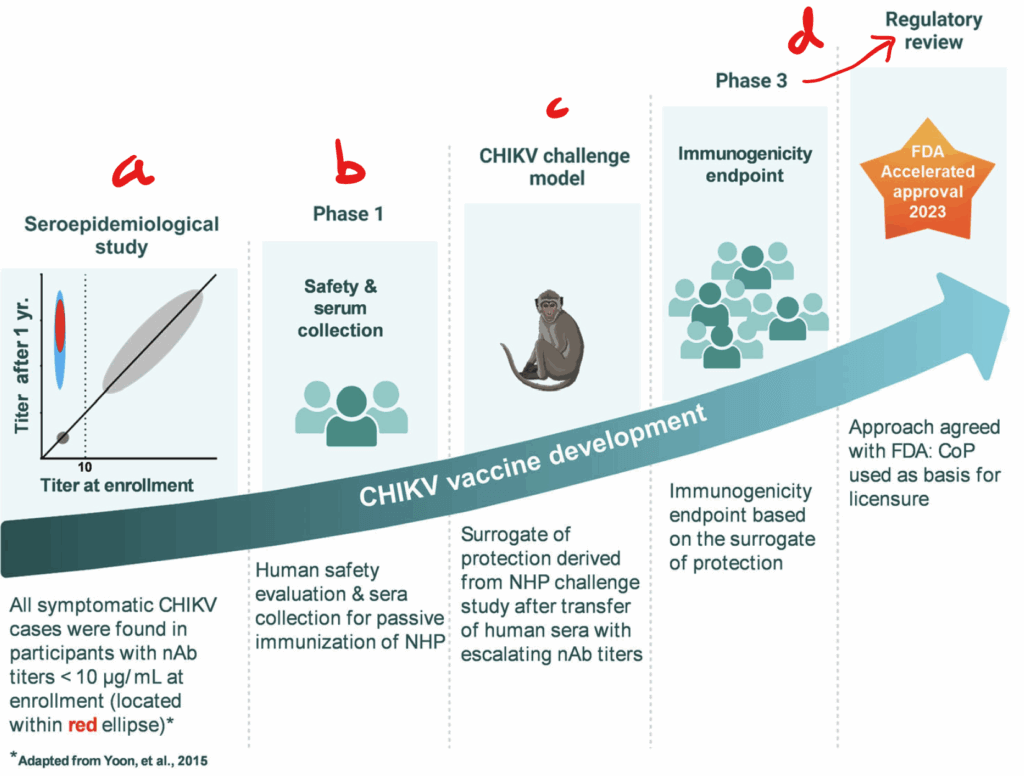
Ways to further leverage this path are possible. As shown in the figure below for the particular case of Chikungunya virus (CHIKV), seroepidemiological data found that all disease cases occurred in subjects who had antibody titers below 10 μg/mL (a). Next, human sera obtained from Ph1 safety studies with an investigational vaccine and containing different levels of neutralizing antibodies (nAbs) were collected (b) and administered (c) to non-human primates (NHP) before challenge with the CHIKV virus. When protection was shown to correlate to the nAb titers, this validation of an antibody titer as a CoP led (d) to approval based on immunogenicity in Phase 3. Clever!
2. Controlled human infection models (CHIMs). Carefully conducted Phase 2 studies in which human volunteers are deliberately exposed to infectious agents are possible for some infections (see Laurens MB, J Infect Dis 2025, doi:10.1093/infdis/jiaf053 if you want to read more about how these studies are safely and ethically conducted). When appropriately conducted, a CHIM can represent a valuable strategy to de-risk vaccine candidates and inform subsequent steps of vaccine development.
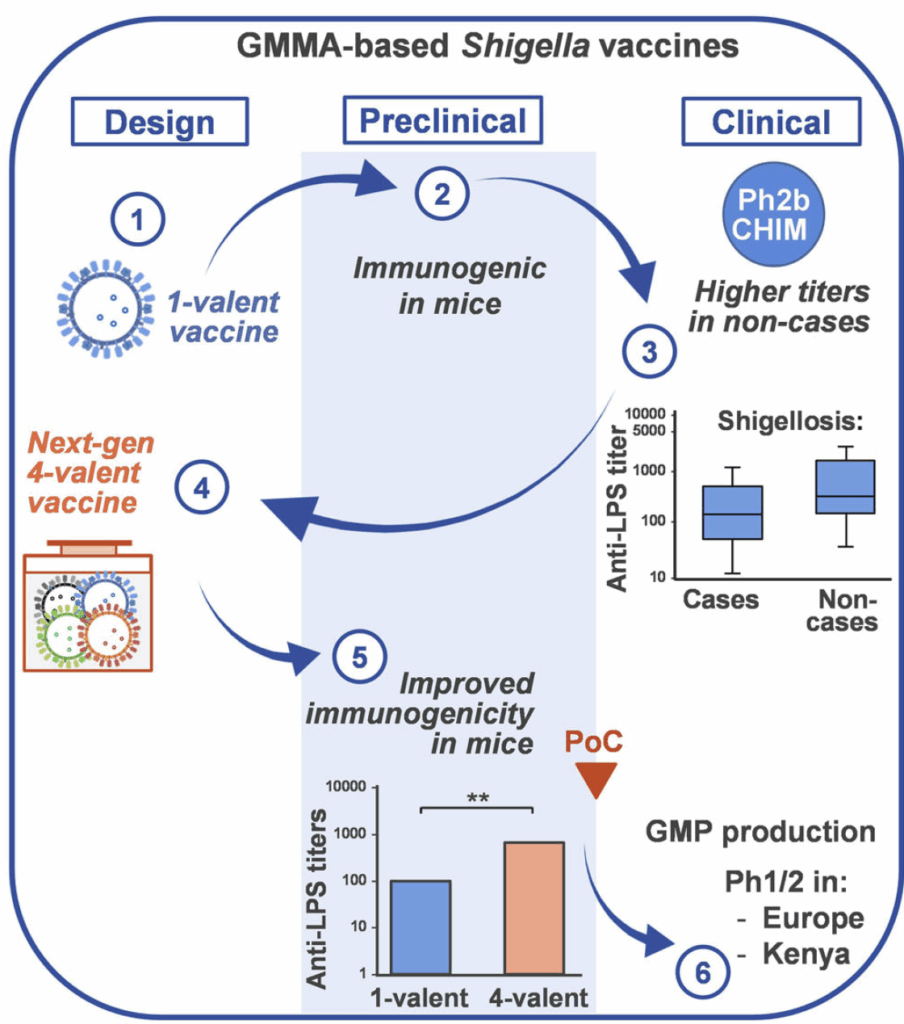
As an example, the authors offer insights into an ongoing project to develop a vaccine for shigellosis, a leading cause of childhood diarrhea. As shown in the figure, (1) an initial 1-valent (one antigen) vaccine for Shigella sonnei was found (2) to be immunogenic in preclinical studies mice. When tested in a Phase 2 CHIM model (3), no protection was observed, but there was a trend for antibody levels to LPS (lipopolysaccharide) to be lower in those who became infected.
This indicated that vaccine candidate had promise! With new insights on titers needed for protection, an improved 4-valent vaccine was created (4). As predicted, the new candidate was found to be more immunogenic in mice (5), thus providing enough confidence to move it into Phase 1 and Phase 2 studies (6). That’s very efficient de-risking!
3. Early, focused studies in higher-risk populations. The final idea discussed by the authors is that development may be de-risked by generating proof of confidence during early-stage clinical studies in carefully selected high-risk subsets of the (ultimate) larger population that is hoped to be protected. As the expected attack rate in this population is far higher compared to the general population, the sample size can be brought down and so the cost of the study. Although this would seem an obvious thing to do, the tricky bit involves identifying that high-risk subset in a timely and efficient manner.
As one example cited in the manuscript, a Phase 3 study of a COVID-19 vaccine in Brazil was efficiently conducted by focusing on health-care professionals caring for COVID-19 patients. As the rate of infection was predicted to be (and actually was) higher in this group that the general population, the study could be smaller.
—
In summary, and with thanks to Vega and her co-authors, it is encouraging to it is encouraging to see that application of early de-risking strategies is possible! Overall, by reducing the overall investment needed to achieve proof of concept for a given candidate, resources could be focused on targets for which preventative strategies still remain elusive.
“An ounce of prevention is definitely worth a pound of cure” and we all win when we have have global, sustainable, and equitable access to life-saving vaccines (see Spee RF 2023 , doi:10.1007/s12471-023-01839-3 for a fun history of that saying).
All best wishes, John and Vega
John H. Rex, MD | Chief Medical Officer, F2G Ltd. | Operating Partner, Advent Life Sciences. Follow me on Twitter: @JohnRex_NewAbx. See past newsletters and subscribe for the future: https://amr.solutions/blog/. All opinions are my own.
Vega Masignani, PhD | CARB-X Alliance Director. | vmasigna@bu.edu. All opinions are my own.
John’s Top Recurring Meetings
Virtual meetings are easy to attend, but regular attendance at annual in-person events is the key to building your network and gaining deeper insight. My personal favorites for such in-person meetings are below. Of particular value for developers, the small meeting format of BEAM’s AMR Conference (March) and GAMRIC (September-October; formerly, the ESCMID-ASM conference series) creates excellent global networking. IDWeek (October) and ECCMID (April) are much larger meetings but also provide opportunities for networking with a substantial, focused audience via their Pipeline sessions. Hope to see you there!
- 1-3 Oct 2025 GAMRIC, the Global AMR Innovators Conference (London, UK). Formerly the ESCMID-ASM Joint Conference on Drug Development for AMR, this meeting series is now in its 10th year and is being continued under the joint sponsorship of CARB-X, ESCMID, BEAM Alliance, GARDP, LifeArc, Boston University, and AMR.Solutions. The ongoing series will continue the successful format of prior meetings with a single-track meeting and substantial networking time (go here to see details of the outstanding 2024 meeting).
- Registration is now open and the agenda can be found at that same link (https://www.gamric.org/). The meeting will be limited to approximately 300 attendees, so please be sure to register promptly to avoid disappointment!
- 19-22 Oct 2025 (Georgia, USA): IDWeek 2025, the annual meeting of the Infectious Diseases Society of America. Go here to register. For those who would like a substantial opportunity to present a product to a large audience (see also adjacent note about ESCMID), note the call for applications to present at an IDWeek Pipeline Session; go here to submit an application for your compound or diagnostic.
- 3-4 Mar 2026 (Basel, Switzerland): The 10th AMR Conference. Sponsored by the BEAM Alliance, the 9th AMR Conference has just concluded and it’s again been an excellent meeting! Please mark your calendar for next year. You can’t register yet, but details will appear here!
- [Abstract submission window now posted] 17-21 April 2026 (Munich, Germany): ESCMID Global 2026, the annual meeting of the European Society for Clinical Microbiology and Infectious Diseases. You can’t register yet, but you can go here for details on the outstanding 2025 meeting. The abstract submission window for 2026 will run 15 October to 26 Nov 2025. For those who would like a substantial opportunity to present a product to a large audience (see also adjacent note about IDWeek), I know that the meeting schedule will again include Pipeline Monday; go here to see details from 2025.
Upcoming meetings of interest to the AMR community:
- 1-3 Oct 2025 GAMRIC, the Global AMR Innovators Conference (London, UK; formerly the ESCMID-ASM Joint Conference on Drug Development for AMR). See list of Top Recurring meetings, above..
- 11-19 Oct 2025 (Annecy, France, residential in-person program): ICARe (Interdisciplinary Course on Antibiotics and Resistance) … and 2025 will be the 9th year for this program. Patrice Courvalin orchestrates content with the support of an all-star scientific committee and faculty. The resulting soup-to-nuts training covers all aspects of antimicrobials, is very intense, and routinely gets rave reviews! Seating is limited, so mark your calendars now if you are interested. Applications are being accepted from 20 Mar to 21 Jun 2025 — go here for more details.
- 9-13 Nov 2025 (Portland, OR, USA): ASM Conference on Biofilms. Go here for details and to register.
- 18-24 Nov 2025 (global, multiple locations): World Antibiotic Awareness Week (WAAW) is convened annually on 18-24 Nov by WHO with national events (e.g., CDC’s US Antibiotic Awareness Week (USAAW); ECDC’s 18 Nov European Antibiotic Awareness Day) occurring around the globe. Details will follow as events become visible.
- [NEW] 20 Nov 2025 (Washington, DC, 9a-5p ET): BARDA Innovation Symposium. BARDA will be showcasing early-stage health security innovations supported by BARDA, including through DRIVe, BARDA Accelerator Network, BARDA Ventures, Blue Knight, and CARB-X. The symposium convenes “a diverse network of early stage companies, government agencies, non dilutive funders, investors, and strategic partners all interested in developing the next generation of medical countermeasures (MCMs).” BARDA has consistently been a very creative funder seeking very diverse types of products … could this be you? Go here for details and to register.
- 19-22 Oct 2025 (Georgia, USA): IDWeek 2025. See list of Top Recurring meetings, above.
- 29-31 Oct 2025 (Bengalaru, India): ASM Global Research Symposium on the One Health Approach to Antimicrobial Resistance (AMR), hosted in partnership with the Centre for Infectious Disease Research (CIDR) at the Indian Institute of Science (IISc). Go here for details and to register.
- [Registration is now open] 28-30 Jan 2026 (Las Vegas, NV, USA): IDSA and ASM have announced a new US-based meeting series entitled IAMRI (Interdisciplinary Meeting on Antimicrobial Resistance and Innovation) and described as a “forum for collaboration and exploration around the latest advances in antimicrobial drug discovery and development.” Go here for more details, to register, and to submit an abstract (deadline for abstracts is 1 Oct 2025).
- 4-5 Feb 2026 (virtual, 8a-noon GMT on both days): Antimicrobial Chemotherapy Conference 2026, sponsored by BSAC and GARDP. Registration here: acc-conference.com. Abstracts are welcomed and can be submitted here; abstract deadline is Friday, 14 November 2025, 17:00 GMT.
- 3-4 Mar 2026 (Basel, Switzerland): The 10th AMR Conference sponsored by the BEAM Alliance. See list of Top Recurring meetings, above.
- 8-13 Mar 2026 (Renaissance Tuscany Il Ciocco, Italy): 2026 Gordon Research Conference (GRC) entitled “Antibacterials of Tomorrow to Combat the Global Threat of Antimicrobial Resistance.” A Gordon Research Seminar (GRS) will be held the weekend before (7-8 Mar) for young doctoral and post-doctoral researchers. Space for the GRS and the GRC is limited; for details and to apply, go here for the GRC and here for the GRS.
- 17-21 April 2026 (Munich, Germany): ESCMID Global 2026, the annual meeting of the European Society for Clinical Microbiology and Infectious Diseases. See Recurring Meetings list, above.
- 4-8 June 2026 (Washington, DC): ASM Microbe, the annual meeting of the American Society for Microbiology. The meeting format is evolving and next year will combine 3 meetings (ASM Health, ASM Applied and Environmental Microbiology, and ASM Mechanism Discovery) into one event. Go here for details.
Self-paced courses, online training materials, and other reference materials:
- OpenWHO: “Antimicrobial Resistance in the environment: key concepts and interventions.” Per the webpage for the course, it will teach you “…why addressing AMR in the environment is essential and gain insights into how action can be taken to prevent and control AMR in the environment at the national level.” This course builds on WHO’s 2024 Guidance on wastewater and solid waste management for manufacturing of antibiotics. For further reading, see also the 25 Sep 2023 newsletter entitled “Manufacturing underpins both access and stewardship: Cefiderocol as a case study” and the 28 Jan 2024 newsletter entitled “EMA Concept Paper: Guidance on manufacturing of phage products”.
- GARDP’s REVIVE website provides an encyclopedia covering a range of R&D terms, recordings of prior GARDP webinars, a variety of viewpoint articles, and more! Check it out!
- GARDP’s https://antibioticdb.com/ is an open-access database of antibacterial agents.
- The CARB-X website provides a range of recordings from its webinars, bootcamps, and more. A bit of browsing would be time well spent!
- British Society for Antimicrobial Chemotherapy offers an eLearning section: Education – The British Society for Antimicrobial Chemotherapy.
- NNF (Novo Nordisk Foundation) have announced their “Challenge Programme 2026 – Unravelling the Pathways of Human Invasive Fungal Diseases. The call seeks applications from EU-centered consortia (global partners are possible) for research in 4 areas: (i) fungal virulence factors, (ii) host-pathogen interactions, (iii) mechanisms of anti-fungal resistance, and (iv) fungal disease markers. Applications are due by 8 Oct 2025. Go here for details.
- ENABLE-2 has continuously open calls for both its Hit-to-Lead program as well as its Hit Identification/Validation incubator. Applicants must be academics and non-profits in Europe due to restrictions from the funders. Applications are evaluated in cycles … see the website for details on current timing for reviews.
- CARB-X will have two calls during 2025 that span two areas: (i) Small molecules for Gram-negatives (the focus is on Pseudomonas aeruginosa) and (ii) Diagnostics for typhoid (the focus is diagnosis of acute infections in 60 minutes or less). See this 26 Feb 2025 newsletter for a discussion of the call and go here for the CARB-X webpage on the call. The first cycle is now closed (it ran16-30 April 2025); the 2nd round will be open 1-12 Dec 2025.
- BARDA’s long-running BAA (Broad Agency Announcement) for medical countermeasures (MCMs) for chemical, biological, radiological, and nuclear (CBRN) threats, pandemic influenza, and emerging infectious diseases is now BAA-23-100-SOL-00004 and offers support for both antibacterial and antifungal agents (as well as antivirals, antitoxins, diagnostics, and more). Note especially these Areas of Interest: Area 3.1 (MDR Bacteria and Biothreat Pathogens), Area 3.2 (MDR Fungal Infections), and Area 7.2 (Antibiotic Resistance Diagnostics for Priority Bacterial Pathogens). Although prior BAAs used a rolling cycle of 4 deadlines/year, the updated BAA released 26 Sep 2023 has a 5-year application period that ends 25 Sep 2028 and is open to applicants regardless of location: BARDA seeks the best science from anywhere in the world! See also this newsletter for further comments on the BAA and its areas of interest.
- HERA Invest was launched August 2023 with €100 million to support innovative EU-based SMEs in the early and late phases of clinical trials. Part of the InvestEU program supporting sustainable investment, innovation, and job creation in Europe, HERA Invest is open for application to companies developing medical countermeasures that address one of the following cross-border health threats: (i) Pathogens with pandemic or epidemic potential, (ii) Chemical, biological, radiological and nuclear (CBRN) threats originating from accidental or deliberate release, and (iii) Antimicrobial resistance (AMR). Non-dilutive venture loans covering up to 50% of investment costs are available. A closing date is not posted insofar as I can see — applications are accepted on a rolling basis; go here for more details.
- The AMR Action Fund is open on an ongoing basis to proposals for funding of Phase 2 / Phase 3 antibacterial therapeutics. Per its charter, the fund prioritizes investment in treatments that address a pathogen prioritized by the WHO, the CDC and/or other public health entities that: (i) are novel (e.g., absence of known cross-resistance, novel targets, new chemical classes, or new mechanisms of action); and/or (ii) have significant differentiated clinical utility (e.g., differentiated innovation that provides clinical value versus standard of care to prescribers and patients, such as safety/tolerability, oral formulation, different spectrum of activity); and (iii) reduce patient mortality. It is also expected that such agents would have the potential to strongly address the likely requirements for delinked Pull incentives such as the UK (NHS England) subscription pilot and the PASTEUR Act in the US. Submit queries to contact@amractionfund.com.
- INCATE (Incubator for Antibacterial Therapies in Europe) is an early-stage funding vehicle supporting innovation vs. drug-resistant bacterial infections. The fund provides advice, community, and non-dilutive funding (€10k in Stage I and up to €250k in Stage II) to support early-stage ventures in creating the evidence and building the team needed to get next-level funding. Details and contacts on their website (https://www.incate.net/).
- These things aren’t sources of funds but would help you develop funding applications
- The Global AMR R&D Hub’s dynamic dashboard (link) summarizes the global clinical development pipeline, incentives for AMR R&D, and investors/investments in AMR R&D.
- Antimicrobial Resistance Research and Innovation in Australia is an actively updated summary that covers Australia’s AMR research and patent landscape. It is provided via collaboration between The Lens (an ambitious project seeking to discover, analyse, and map global innovation knowledge) and CSIRO (Commonwealth Scientific and Industrial Research Organisation, an Australian Government agency responsible for scientific research). Lots to explore here!
- Diagnostic developers would find valuable guidance in this 6-part series on in vitro diagnostic (IVD) development. Sponsored by CARB-X, C-CAMP, and FIND, it pulls together real-life insights into a succinct set of tutorials.
- In addition to the lists provided by the Global AMR R&D Hub, you might also be interested in my most current lists of R&D incentives (link) and priority pathogens (link).