17 Sep 2024 update: This is now the first of a 3-part newsletter series! See also part 2 (“R&D Implications: Global Burden of Disease is 28% Infectious!“) and part 3 (17 Sep 2024: “#AMRSOS! AMR could worsen, killing 39m during 2025-2050”).
Dear All,
There are days when it is hard to keep up! Not only did we have the release today of two amazing sets of RFPs from NIAID and BARDA (Vaccines! Therapeutics! Diagnostics! Bacteria! Fungi! Viruses! See this newsletter!) but we also have the impressive GRAM (Global Research on Antimicrobial Resistance) report by Murray et al. Here are the details:
- The paper: Murray CJL, Ikuta KS, Sharara F, Swetschinski L, Robles Aguilar G, Gray A, et al. Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. The Lancet: https://doi.org/10.1016/S0140-6736(21)02724-0.
- The key message: “at least 1.27 million deaths per year are directly attributable to AMR”
- The details (well, some of the details — I quote here from the abstract):
- “We estimated deaths and disability-adjusted life-years (DALYs) attributable to and associated with bacterial AMR for 23 pathogens and 88 pathogen–drug combinations in 204 countries and territories in 2019.
- “We obtained data from systematic literature reviews, hospital systems, surveillance systems, and other sources, covering 471 million individual records or isolates and 7585 study-location-years.
- “On the basis of our predictive statistical models, there were an estimated 4·95 million (3·62–6·57) deaths associated with bacterial AMR in 2019, including 1·27 million (95% UI 0·911–1·71) deaths attributable to bacterial AMR.
- “At the regional level, we estimated the all-age death rate attributable to resistance to be highest in western sub-Saharan Africa, at 27·3 deaths per 100 000 (20·9–35·3), and lowest in Australasia, at 6·5 deaths (4·3–9·4) per 100 000.
- “Lower respiratory infections accounted for more than 1·5 million deaths associated with resistance in 2019, making it the most burdensome infectious syndrome.
- “The six leading pathogens for deaths associated with resistance (Escherichia coli, followed by Staphylococcus aureus, Klebsiella pneumoniae, Streptococcus pneumoniae, Acinetobacter baumannii, and Pseudomonas aeruginosa) were responsible for 929 000 (660 000–1 270 000) deaths attributable to AMR and 3·57 million (2·62–4·78) deaths associated with AMR in 2019.
- “One pathogen–drug combination, methicillin-resistant S aureus, caused more than 100 000 deaths attributable to AMR in 2019, while six more each caused 50 000–100 000 deaths: multidrug-resistant excluding extensively drug-resistant tuberculosis, third-generation cephalosporin-resistant E coli, carbapenem-resistant A baumannii, fluoroquinolone-resistant E coli, carbapenem-resistant K pneumoniae, and third-generation cephalosporin-resistant K pneumoniae.”
- The context: These are the most comprehensive global estimates of AMR burden since the 2016 estimates by the UK AMR Review and the magnitude of mortality due to AMR is similar (see discussion at the bottom of page 21 of the paper).
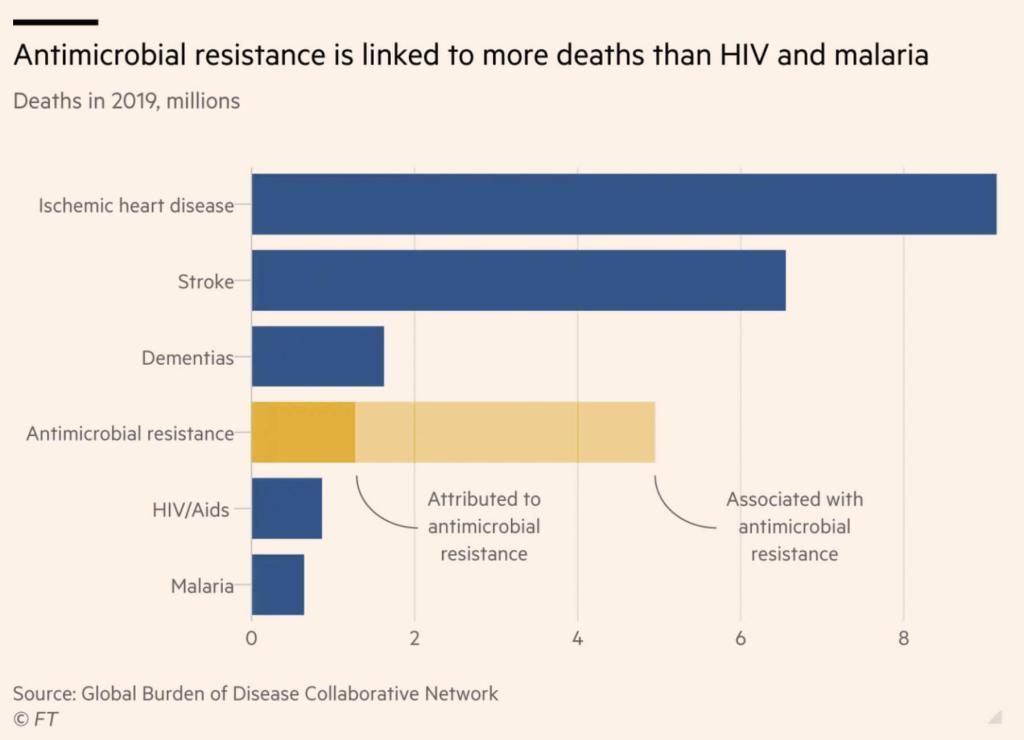
- The graphics (31 Jan 2022 addendum): I show one graphic a bit further below, but Andrew Jack at the FT has done a superb job with graphics from this report in his 19 Jan 2022 commentary. This chart in particular delivers a sharp message:
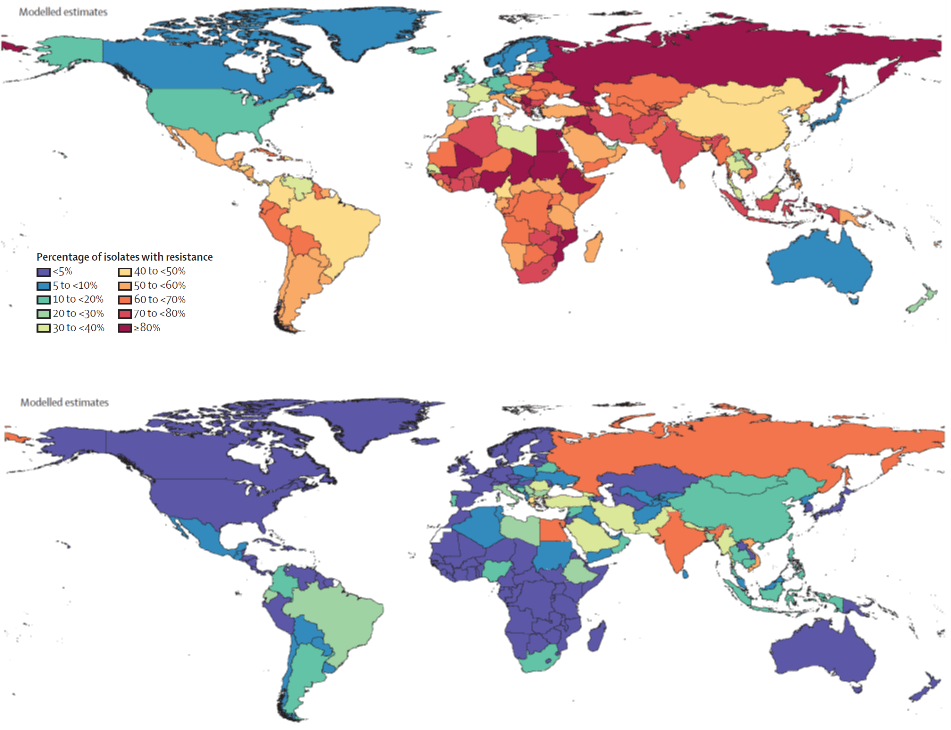
- Another key message: No one is safe: There are some really scary figures showing spread of highly resistant organisms. I show here the pattern of K. pneumoniae resistant to 3rd-generation cephalosporins (upper, these are the preferred first-line drugs) and carbapenems (lower, these are the backup agents … when these fail, you are in trouble). Purple is lowest rate of resistance, blue-green is < 50%, yellow-red is > 50%. As you can see, the resistant pathogens are steadily spreading:
Wow! Wow! WOW! We’ll be referring to this one for years. MANY thanks to the impressive array of project sponsors:
- Institute for Health Metrics and Evaluation (IHME) (@IHME_UW)
- University of Oxford (@UniofOxford)
- Wellcome Trust (@WellcomeTrust), (@Wellcome_AMR)
- The Fleming Fund (@FlemingFund)
- UK Department of Health and Social Care (DHSC) (@DHSCgovuk),
- Global Health Security, DHSC (@UKgovGHS)
- The Bill and Melinda Gates Foundation (@gatesfoundation),
- The Lancet (@TheLancet)
- Dame Sally Davies, UK Special Envoy on Antimicrobial Resistance (@UKAMREnvoy)
And, of course, the core message is that we’re in trouble. The antibacterial pipeline is thin (17 Jan 2022 newsletter), R&D for new antibacterial takes years (Dheman 2020 CID and the accompanying Rex-Outterson editorial), and (finally!) the economics of new antibiotics are horrid and require a fix in the form of substantial Pull Incentives paid to innovators upon approval of meaningful new therapies.
Our work is cut out for us! #AMRSOS! Get going!
All best wishes, –jr
John H. Rex, MD | Chief Medical Officer, F2G Ltd. | Operating Partner, Advent Life Sciences. Follow me on Twitter: @JohnRex_NewAbx. See past newsletters and subscribe for the future: https://amr.solutions/blog/. All opinions are my own.
Current funding opportunities (most current list is here):
- NIAID has released a four-pronged BAA (Broad Agency Announcement (HHS-NIH-NIAID-BAA2022-1) that covers therapeutics (antibacterial, antifungal, antiviral), vaccines (again, all 3 areas), and diagnostics. Lots of possibilities! The due date is 18 Mar 2022.
- BARDA’s RFP to support new antibiotics for Yersinia pestis, Francisella tularensis, Burkholderia pseudomallei is open through 6 April 2022. The RFP offers from funding from LO to Phase 2. Go here for the details.
- JPIAMR’s 14th call is now open. Entitled “Disrupting drug resistance using innovative design”, the call seeks consortia that would seek to “improve the treatment of bacterial and fungal infections (including co-infection) and/or the prevention of the emergence/spread of resistance in humans, animals or plants through the improvement of the efficacy, specificity, delivery, combinations and/or repurposing of drugs and plant protection agents.” Bacteria, fungi, human health, animal health, and plant health are all in scope! Pre-proposals are due 8 Mar 2022; full proposals would be due 5 July 2022. Go here for details.
- The AMR Action Fund is now open to proposals for funding of Phase 2 / Phase 3 antibacterial therapeutics. Per its charter, the fund prioritizes investment in treatments that address a pathogen prioritized by the WHO, the CDC and/or other public health entities that: (i) are novel (e.g., absence of known cross-resistance, novel targets, new chemical classes, or new mechanisms of action); and/or (ii) have significant differentiated clinical utility (e.g., differentiated innovation that provides clinical value versus standard of care to prescribers and patients, such as safety/tolerability, oral formulation, different spectrum of activity); and (iii) reduce patient mortality. It is also expected that such agents would have the potential to strongly address the likely requirements for delinked Pull incentives such as the UK (NHS England) subscription pilot and the PASTEUR Act in the US. Submit queries to contact@amractionfund.com.
- INCATE (Incubator for Antibacterial Therapies in Europe) is a newly launched early-stage funding vehicle. Details are still coming into focus, but per comments on 25 Aug 2021 at the BIOCOM conference, their goal is to support ~4 companies per year with about $250k/company. Contact details are on their website (https://www.incate.net/).
- CARB-X recently announced that their existing resources will be reserved to fund their existing portfolio (more than 80 total awards, and counting, as they include contracting from prior rounds). New rounds from CARB-X will occur only after new funding is obtained in 2021.
- It’s not a funder, but AiCuris’ AiCubator offers incubator support to very early stage projects. Read more about it here.
- The Global AMR R&D Hub’s dynamic dashboard (link) summarizes the global clinical development pipeline, incentives for AMR R&D, and investors/investments in AMR R&D.
- In addition to the lists provided by the Global AMR R&D Hub, you might also be interested in my most current lists of R&D incentives (link) and priority pathogens (link).
Upcoming meetings of interest to the AMR community (most current list is here):
- [If you missed it, you can now watch the video] 8 Dec: “The New Winds Pushing and Pulling Antibacterial Development.” This was a GREAT program that featured talks from the UK team behind the NHS “Netflix” pilot, Kevin Outterson’s recently released report documenting the need for global Pull incentives to have a value of $2.2 – 4.8b, and speakers covering PASTEUR and work in the EU on pull incentives. The video is here — please make time to listen to this program!
- 26 Jan 2022 (virtual, 2-3.30p CET): REVIVE (GARDP) Webinar: New technologies and strategies to overcome the challenges of sexually transmitted infections. Moderated by Amir Schroufi and Remco Peters, the program will covers strategies for managing STDs with a particular focus on the developing world. Go here to register.
- 2-3 Feb 2022 (virtual): 10th Advances Against Aspergillosis and Mucormycosis. Registration closes on 30 Jan 2022. Go here for details.
- 2-3 Feb 2022 (virtual): Antimicrobial Chemotherapy Virtual Conference jointly organised by GARDP with the British Society for Antimicrobial Chemotherapy (BSAC), Center for Disease Dynamics, Economics & Policy (CDDEP) and the Indian Council of Medical Research (ICMR). Click here for details.
- [NEW] 4 Feb 2022 (virtual, 5-6.30p GMT): Launch of the GRAM (Global Research on Antimicrobial Resistance) report. Sponsored by the Institute for Health Metrics and Evaluation, the University of Oxford, the Fleming Fund, the Bill & Melinda Gates Foundation and Wellcome Trust, this report by Murray et al. is based on 471 million individual records or isolates and 7585 study-location-years’ worth of data and shows that at least 1.27 million deaths per year are directly attributable to AMR. Amazing stuff! #AMRSOS! Go here to register. If you miss it, a post-event recording will be available.
- 7 Feb 2022 (virtual, 10a-11.30a and 3:30p-5p CET): 2-part webinar entitled Antimicrobial Consumption & Use – Data for Action as part of the WHO Global Webinar Series. Be sure to register for both session 1 and session 2!
- 3-6 Mar 2022 (Albuquerque, New Mexico): Biannual meeting of the MSGERC (Mycoses Study Group Education and Research Consortium). Details are here.
- 6-11 Mar 2022 (Il Ciocco, Tuscany): Gordon Research Conference entitled “New Antibacterial Discovery and Development”. Go here for details, go here for the linked 5-6 Mar Gordon Research Seminar that precedes it.
- 9 Mar 2022 (virtual, and in-person): BioInfect Conference, Alderley Park, UK (near Manchester). This long-running Bionow-sponsored annual conference draws a very strong audience. Go here for details.
- 7-8 Apr 2022 (Basel and in person, we hope): The 6th edition of the annual AMR conference sponsored by the BEAM Alliance, CARB-X, the Novo REPAIR Impact Fund, the IMI Accelerator, and the European Biotechnology Network. Go here for the hold-the-date page and a way to be kept informed about the meeting.
- 9-13 May 2022 (Athens and online): 40th Annual Meeting of the European Society for Paediatric Infectious Diseases, Go here for details.
- 20-24 Sep 2022 (New Delhi): 21st Congress of the International Society for Human and Animal Mycology (ISHAM). Go here for details.
- 25-28 Oct 2022 (Stellenbosch, South Africa): The University of Cape Town’s H3D Research Centre will celebrate its 10th anniversary with a symposium covering the Centre’s research on Malaria, TB, Neglected Tropical Diseases, and AMR. Go here to register.