Dear All:
CDC has today announced $9m in funding for more than 20 new projects focused on slowing or combating antimicrobial resistance. Part of the CDC’s Antibiotic Resistance Solutions Initiative, these projects span a broad range that includes surveillance (C. auris, antibiotic resistance in a watershed, antibiotic resistance in poultry farms), diagnostics (POC tools, what’s in hospital sewage discharge?), fellowship training in stewardship, and much, much more. The full list with some details can be be found online at the link above and I’ve produced a high-level summary just below my signature in which I broadly classify the projects for ease of review.
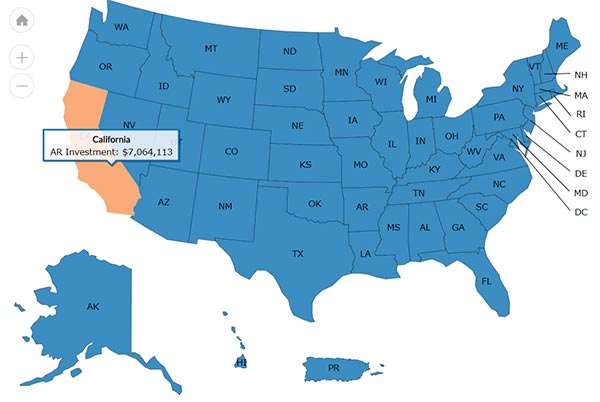
Combined with the 2016 investments, CDC’s AR Solutions Initiative has awarded more than $24 million to investigators through a broad agency announcement. There’s a neat online map that shows how this has been spread across the US — I show here the map with California highlighted:
It’s great to see our US Gov’t partners so deeply and well engaged in addressing the challenge of AMR. I’m particularly impressed by the breadth of projects … from microbiome to clinical investigations, CDC has really cast a broad net. Go CDC!
All best wishes, –jr
John H. Rex, MD | Chief Medical Officer, F2G Ltd. | Expert-in-Residence, Wellcome Trust. Follow me on Twitter: @JohnRex_NewAbx. See past newsletters and subscribe for the future: https://13.43.35.2/blog/
List of projects newly funded by CDC:
Microbiome
- Baylor College of Medicine: Cross-validation of human fecal minibioreactor arrays and humanized microbiota mice as complementary pre-clinical models of the GI (gastrointestinal) microbiome
- Regents of the University of Michigan: Microbiome disruption and Enterobacteriaceae dominance as a risk factor for sepsis in intensive care patients
Diagnostics & Bioinformatics
- Children’s Hospital Oakland Research Institute (CHORI) at the University of California San Francisco: Rapid assays to detect Neisseria gonorrhea antibiotic resistance at the point of care
- Emory University: Computational methods for culture-independent disambiguation of wgMLST types in biological samples with multiple related bacterial strains
- J. Craig Venter Institute (JCVI): Improved bioinformatics tools for detection and characterization of antimicrobial resistance in public health
- University of Mississippi Medical Center: Comparison of methods for detecting recombination in bacterial whole genome sequences
Epidemiology
- Rutgers, the State University of New Jersey: Rapid identification and analysis of transmission of the emerging pathogen Candida auris
- The Ohio State University: Preventing the dissemination of CRE from healthcare facilities into surface waters in the US (continuation request)
- The Rector and Visitors of the University of Virginia: Understanding the microbiologic dynamics of Carbapenemase-producing organisms in hospital wastewater premise plumbing
- The University of Georgia: The prevalence and diversity of antibiotic resistant bacteria in a mixed-use watershed
- University of Alabama at Birmingham: Sentinel surveillance for Macrolide-resistant Mycoplasma pneumoniae at select sites in the United States
Food agriculture
- Georgia Tech Applied Research Corporation (GTARC): Antibiotic resistance in concentrated poultry feeding operations: Impacts on environmental waters
- University of Georgia Research Foundation, Inc.: Azole resistance in agricultural settings
Training
- Infectious Diseases Society of America (IDSA): Infectious Diseases Fellowships to drive innovative education and approaches in antibiotic resistance, antibiotic stewardship and public health (AR/AS Public Health Innovation Fellowships)
- OpGen, Inc.: Highly accessible system for infection control and antimicrobial stewardship in resource limited settings
- The Children’s Hospital of Philadelphia (CHOP): Perinatal antibiotics and weight gain in childhood
- Translational Genomics Research Institute (TGen): Considering homologous and non-homologous recombination in outbreak analysis
Clinical investigations
- Cleveland VA Medical Research and Education Foundation: Natural history of Clostridium difficile colonization
- Department of Research & Evaluation, Kaiser Permanente Southern California: Prenatal antibiotic use and body weight in children
- Georgia Tech Applied Research Corporation (GTARC): Optimization of therapeutic strategies to manage polymicrobial CF lung infections: Clinical assessment
- University of Arizona: Reducing antibacterial use in patients with coccidioidomycosis
- University of Maryland, Baltimore: Implementation of a novel strategy to prevent Staphylococcus aureus (SA) acquisition and hence invasive SA infection in community-based nursing homes: Feasibility and pilot to guide a multicenter stepped wedge cluster trial
- Washington University: Double blinded, randomized controlled Trial of Oral vancomycin versus placebo in hospitalized patients with diarrhea and stool toXin NEGative but nucleic acid amplification test positive for toxigenic Clostridium difficile (TOX NEG trial)
Upcoming meetings of interest to the AMR community:
- 29 Oct-1 Nov 2017 (Santa Fe): Keystone Symposium – Antimicrobials and Resistance: Opportunities and Challenges
- 3 Nov 2017 (no specific location): One Health Day
- 6 Nov 2017 (Boston): BAARN (Boston-Area Antimicrobial Resistance Network), Annual Meeting for 2017
- [NEW] 7 Nov 2017 (Washington, DC): FDA VRBPAC (Vaccines & Related Biologic Products) AdComm on the clinical development plan for Pfizer’s investigational Staphylococcus aureus vaccine intended for pre-surgical prophylaxis in elective orthopedic surgical population
- 7-8 Nov 2017 (Washington, DC): BARDA Industry Days
- 11-19 Nov 2017 (Annecy, France): International Course on Antibiotics and Resistance (ICARE)
- 13-19 Nov 2017 WHO’s World Antibiotic Awareness Week
- 15 Nov 2017 (London): BSAC: AMR Market Lounges. Networking day.
- 20 Nov 2017 (week of, China): UK-China Newton Fund Workshop: Antimicrobial Resistance Centre Partnerships Initiative.
- 20 Nov 2017 (London): Early Career Researcher Workshop on Diagnostics for Antimicrobial Resistance.
- 24-27 Nov 2017 (Taipei): 30th International Congress of Chemotherapy & Infection (ICC)
- 12-14 Feb 2018 (Baltimore): ASM Biothreats Conference
- 11-16 Mar 2018 (Ventura Beach): Gordon Research Conference on Antibacterial Discovery
- 21-24 Apr 2018 (Madrid): ECCMID
- 7-11 Jun 2018 (Atlanta): ASM Microbe
- 22-27 Jul 2018 (Bryant University, Smithfield, RI): Gordon Research Conference on Drug Resistance for Cancer, Infectious Disease and Agriculture